What are some of the causes of painful sex?
Some common complaints we see include:
- Vaginal and vulval skin issues such as dryness, thinning and splitting, or dermatological conditions such as eczema, psoriasis, dermatitis, lichen sclerosus (stiff white-coloured skin in the vulva)
- Endometriosis – deep pain with intercourse, significant pain with periods, pain with bowel movements at period time, pain between periods, very heavy bleeding and clots
- Pelvic floor muscle tightness – sensation like a ‘ball’ in the rectum
- Nerve pain after injury, surgery or having a baby – burning, tingling or shooting pain, worse with sitting
- Mechanical pain due to a musculoskeletal issue with the joints or muscles of the pelvis or hips
- Bacterial, fungal or sexually transmitted infections such as genital warts or herpes, recurrent thrush (curds and whey-type discharge), which can be itchy and painful
How do you treat the symptoms of painful sex?
Intercourse pain can contribute to significant psychological distress, a fear of intercourse and avoiding sex all together. This can impact on self-esteem, relationships and your mental health.
At WHRIA we provide psychological services including Cognitive Behavioural Therapy (CBT), clinical hypnotherapy, and couples counselling to help you with this important aspect of your care.
How do I know what is causing painful sex?
During your appointment, we may talk through your answers to the following questions to determine the best treatment plan for your specific issues.
For women:
1. Do you feel pain closer to the surface, near the vaginal opening or vulva with touch or penetration?
This may lead us to identify:
- Vaginal and vulval skin issues – dryness and splitting, dermatological conditions such as eczema, psoriasis, dermatitis, lichen sclerosus
- Vaginal thinning (atrophy) – dryness, burning, and itchiness
- Recurrent fungal, bacterial or viral infections
- Nerve pain after injury, surgery or having a baby
- Pudendal nerve pain (pudendal neuralgia) if the pain is worse when sitting and at the end of the day – typically if you feel pain in the anus and rectum, perineum, vagina, labia and clitoris / penis
- Pelvic floor muscles – if your muscles are tight, or unable to relax or ‘switch off’
- Bladder issues such as Painful Bladder Syndrome, overactive bladder, recurrent infections, or cystitis-like symptoms without infection – if you experience stinging or burning during urination, or have to urinate very often in the day and night
- Being born with an abnormality (this is rare)
If you anticipate pain and are worried about having sex due to pain, this can compound the problem and tighten your pelvic floor muscles, which then produce their own pain and amplify your original pain.
What causes vaginal thinning?
Vaginal thinning is caused by an under-supply of oestrogen, and results in reduced hydration and thickness of the protective mucosa.
In younger women, vaginal thinning can be associated with polycystic ovaries (PCOS), eating disorders, low body weight, post-cancer treatment, early menopause or high level athletic training.
As you get older, vaginal thinning is a normal ageing process after menopause but can be worse in some women who may also have had treatment for cancer. It requires an appropriate daily skin care regime.
Sometimes, prolonged use of the Pill, injected or rod-type hormonal contraceptives may also lead to an under supply of oestrogen.
2. Do you feel deeper pain in your pelvis, low back or abdomen?
This may lead us to identify:
- Endometriosis – if you have deep pain with intercourse, significant pain with periods, pain with bowel movements at period time, pain between periods, very heavy bleeding and clots
- Trauma after surgery or having a baby, from a fall or injury, or psychological trauma
- Pelvic scarring or adhesions – after an infection, surgery or radiation treatment
- Bowel issues such as IBS (Irritable Bowel Syndrome), constipation and straining, loose stool
- Bladder issues such as recurrent infection or Painful Bladder Syndrome
- Sacroiliac or hip joint pain if you have aching in the low back, hips, pelvis or low abdomen, limping
- Pelvic floor muscle pain due to over contracting muscles
- Pudendal nerve pain (pudendal neuralgia) if the pain is worse when sitting and at the end of the day
- Pelvic infection – typically you’ll also have other indicators of infection such as fever, diarrhoea, cramping, coloured or smelly discharge, stinging urination or a history of unprotected sex
For women and men
3. Is it related to the position of sex?
If you experience pain in your pelvis due to the position or the movements involved in having sex, this could indicate a musculoskeletal issue and there may be a problem with the muscles, joints and soft tissues of your pelvis, hips and back.
This can occur in both women and men, and is thought to be fairly common. Pain with movement can often occur in addition to another pain, or in response to another pain because pelvic muscles tighten as a part of the normal human protective response. Manual therapy including pelvic floor physiotherapy, osteopathy and acupuncture are options provided at WHRIA as a part of your holistic care.
For men
4. Does pain occur during or after intercourse?
This may indicate pudendal nerve pain (pudendal neuralgia). The pain may be associated with sex and can be experienced in the scrotum, anus, rectum or testes. It can also occur after sex and is perceived as pain or numbness in the penis.
Other potential causes for men:
- Recurrent fungal, bacterial or viral infections
- Bladder issues such as Painful Bladder Syndrome or recurrent infection
- Prostate issues
- Pelvic floor muscles: tight, bulky and over-contracted or spasming muscles, inability to relax or ‘switch off’ the muscles. These over-contracting muscles can produce their own pain which can amplify the original pain
If you have a specific enquiry for our WHRIA specialists
Click HereHow is painful sex treated at WHRIA?
We look at all aspects that contribute to your pain so we will take a thorough history, and carry out an examination and tests as required, along with mental fitness questionnaires.
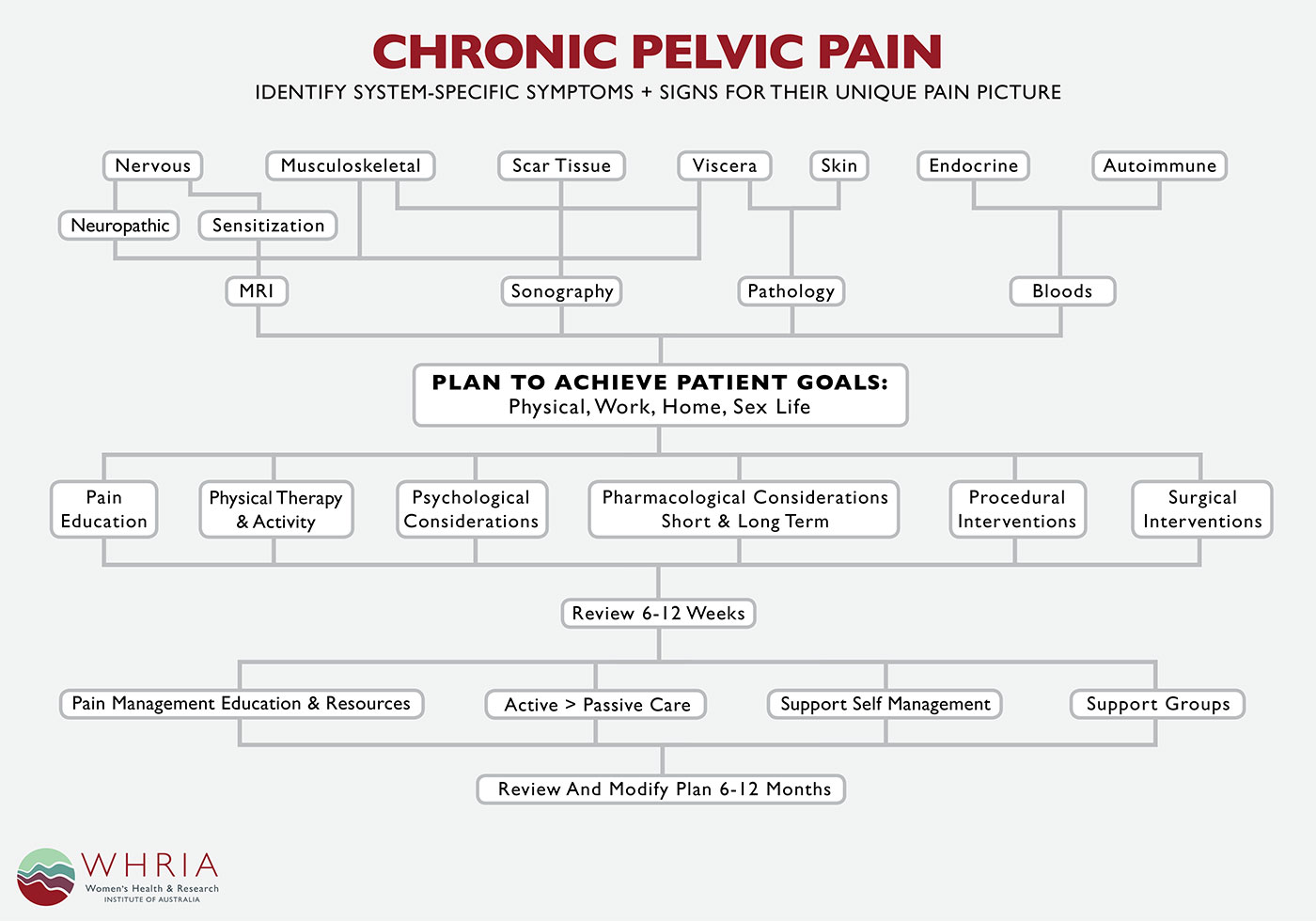
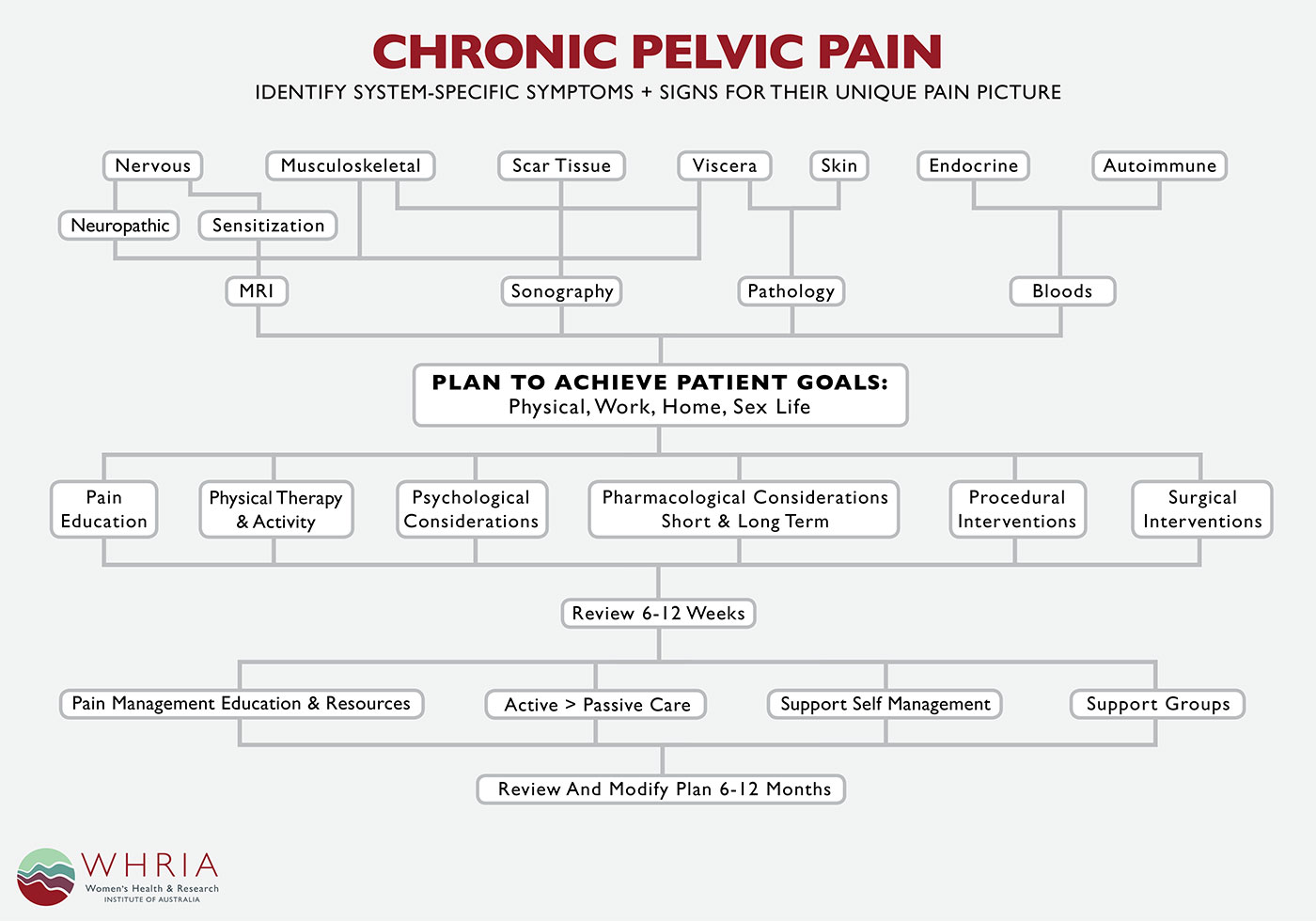
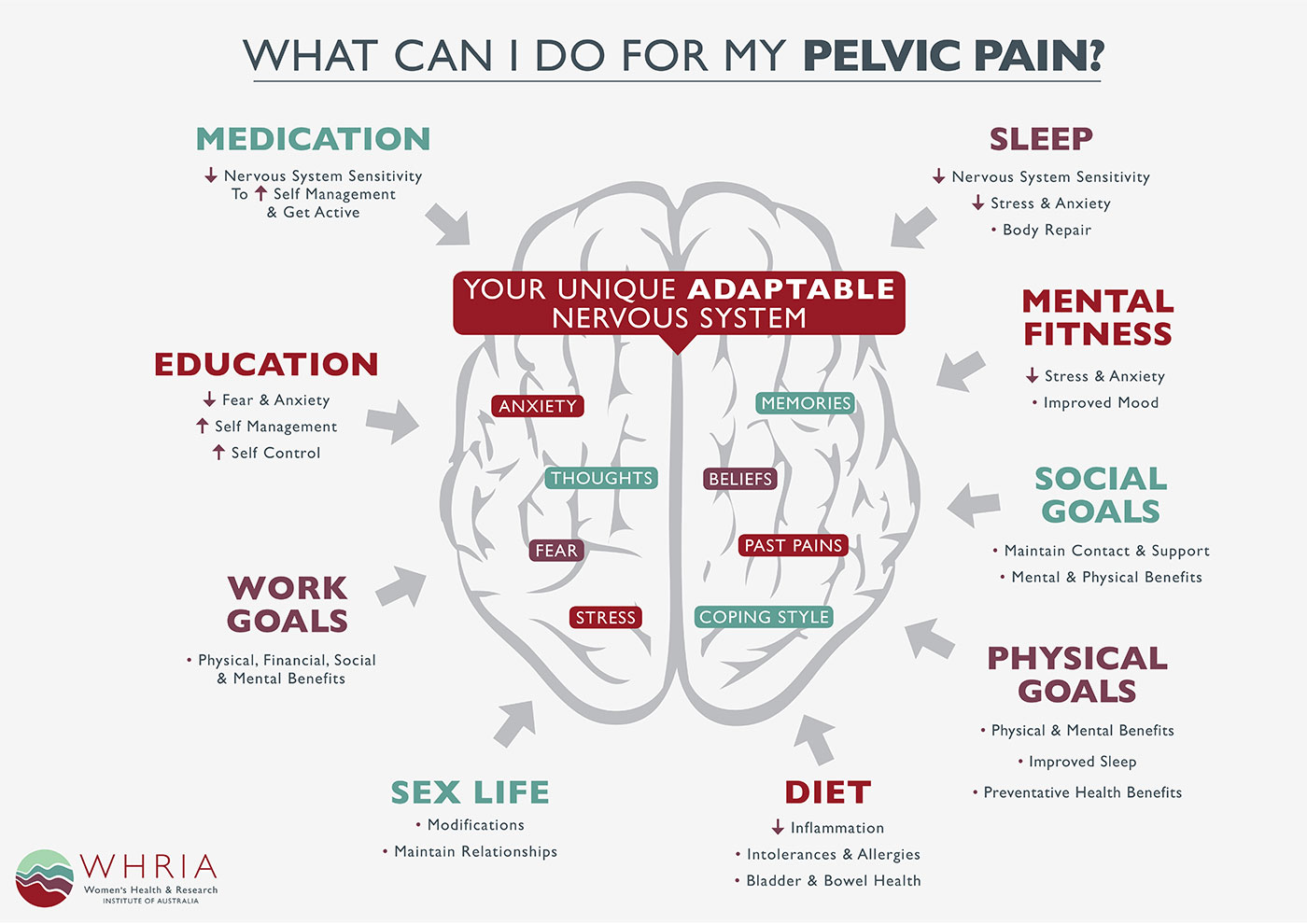
This Chronic Pelvic Pain diagram explains the services available (click to enlarge).
Holistic approach
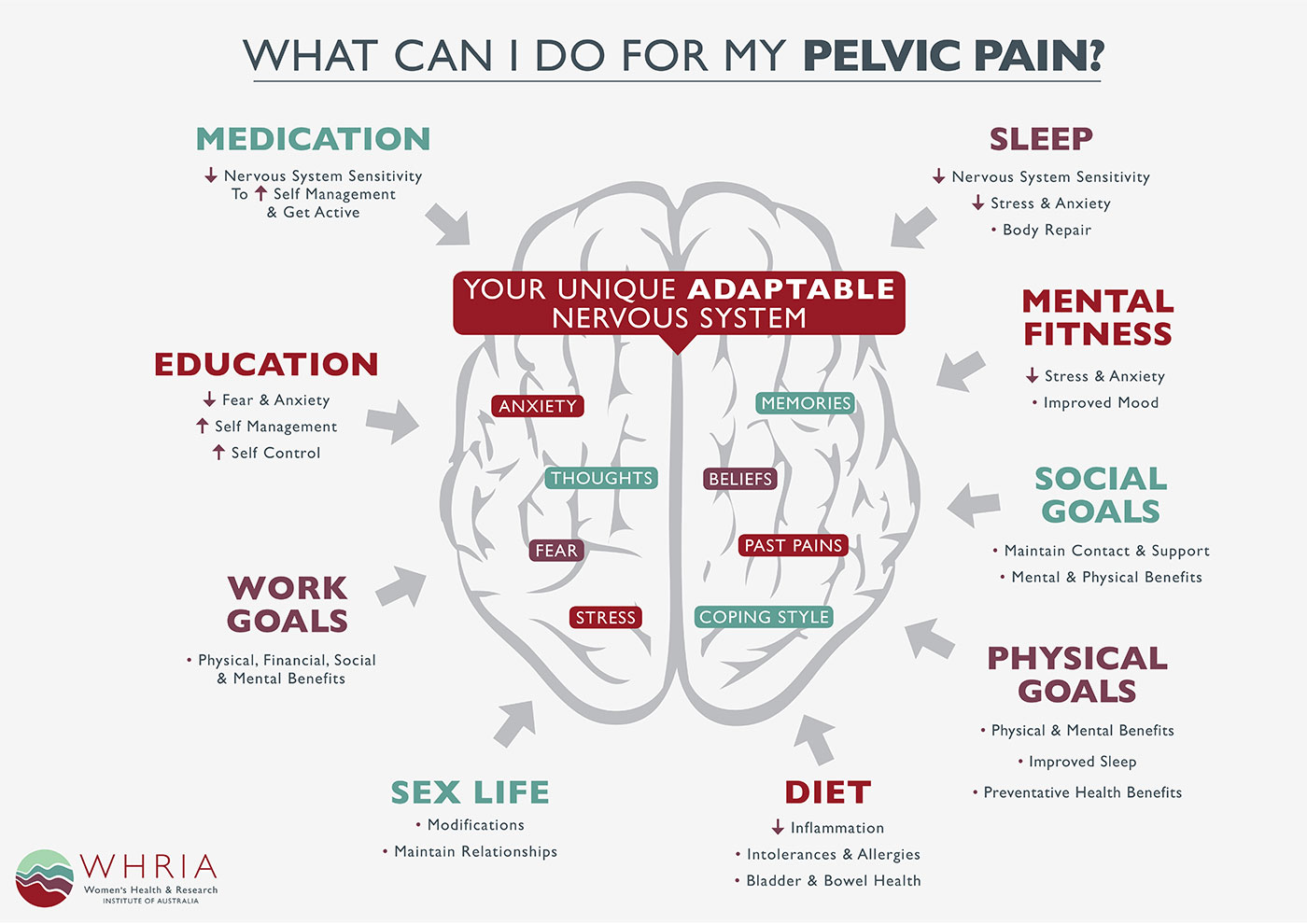
Pain is a very individual experience and is strongly linked to your emotions. Emotions are thought to be a significant modulator of pain via both nerve and hormonal effects. So it is important to consider all aspects of pain, including the mind.
Studies using brain imaging have shown that anticipating pain or being fearful or worried about feeling pain can also trigger pain, or increase another pain. Addressing your mental fitness and the way you cope with or respond to pain is an important aspect of your care at WHRIA, and we provide psychology, hypnotherapy and counselling to help you, in conjunction with your physical care.
Conservative management
We can address the underlying physical issues contributing to painful sex with treatment, education and self-management. Your conservative management treatment plan at WHRIA may include:
- Physiotherapy management including internal and external stretches and relaxation exercises you can do at home
- Osteopathic manual therapy and home management (movement and stretches for external muscles and joints)
- Bladder and bowel management
- Medication (tablets or creams)
- Hormonal therapies including herbal medicine (tablets, creams or patches)
- Acupuncture and Traditional Chinese Herbal Medicine
- Vaginal and vulval skin treatments and self-care education
- Lifestyle modifications for your home, work, social and sex life
- Psychological practical pain-management skills
- Pain education
Procedures for painful sex
Most patients improve with conservative management, however we do provide the following services if required:
- Musculoskeletal injections, such as cortisone for tendinitis or joint inflammation
- Pelvic floor muscle over-contraction treatment with BOTOX / Botulinum Toxin Type A injections
- Fractional CO2 Laser Therapy for vulvo-vaginal atrophy
- Pulsed Radio Frequency for nerve pain
- Gynaecological surgery including minimally invasive procedures such as laparoscopy for resection of endometriosis
- Pudendal nerve block may be helpful for diagnosis
Make an appointment at WHRIA
Talk with your GP about the most appropriate WHRIA service for your pain. If you wish to see one of our doctors you will need a referral.
You may prefer to start with one of the Allied Health team, where no referral is required. All WHRIA practitioners are trained to recognise when you will benefit from the care of more than just one service, and this can be discussed as part of your consultation.
WHRIA specialists and practitioners for painful sex consultations
- Vaginal and vulval skin symptoms – Dr Yasmin Tan, Gynaecologist and Ultrasound specialist
- Low oestrogen or hormonal symptoms – Dr Yasmin Tan or Professor John Eden
- Nerve pain symptoms, post-surgery or trauma – Dr Jason Chow or Professor Thierry Vancaillie, Pain Medicine Specialists and Gynaecologists
- Pelvic floor muscle symptoms – Sherin Jarvis or Donna Namdaram Reynolds, Pelvic Floor Physiotherapists
- SIJ, hip or lower back problems – Amy Corcoran or Liz Howard, Osteopaths
- Acupuncture and herbal medicine, for recent pain, recovering from trauma, surgery or birth – Bernice Lowe
More information
If you’d like more information you can view the health information fact sheets below or browse our Health Information page.
If you have a specific enquiry for our WHRIA specialists
Click Here